Osteomalacia: Understanding Types, Causes, Symptoms, Prevention, Coping Strategies, and Treatment;
A Holistic Approach:
Introduction:
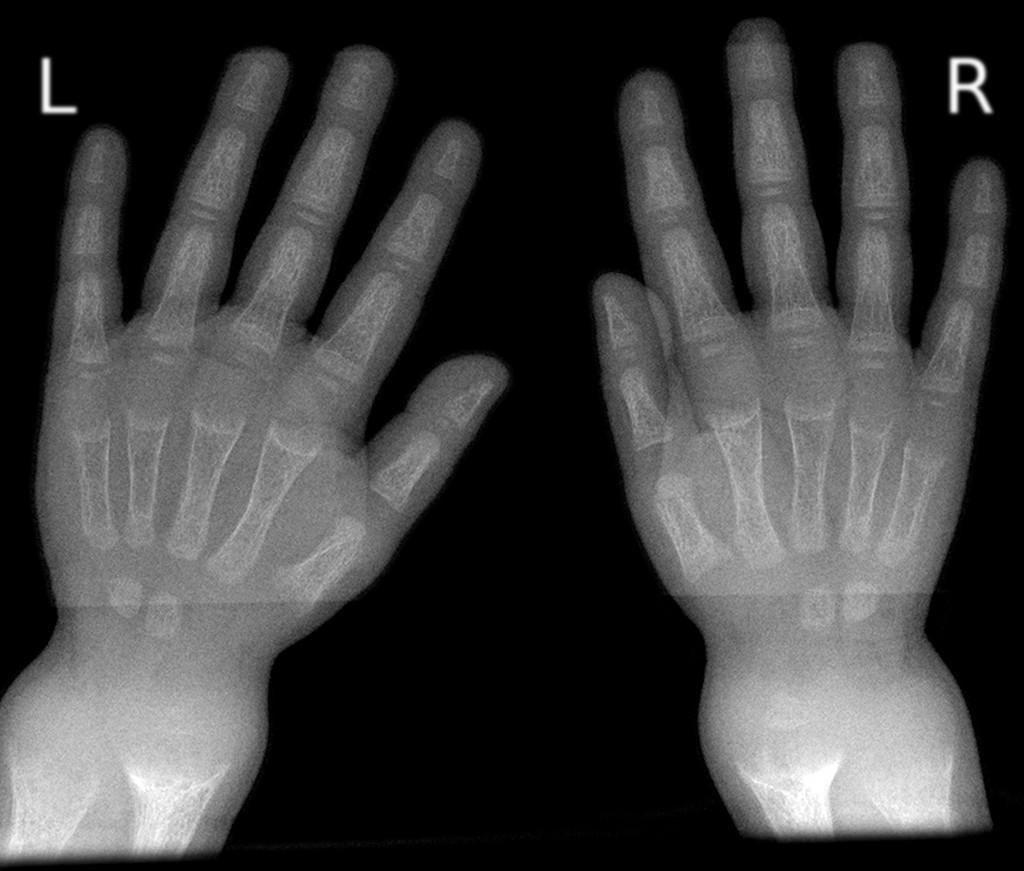
Osteomalacia, a metabolic bone disorder, is characterized by the softening and weakening of bones due to a deficiency of vitamin D or problems with its metabolism. It can lead to bone pain, fractures, and overall decreased bone strength. In this article, we will explore the different types of osteomalacia, the underlying reasons behind it, common symptoms, strategies for prevention and coping through lifestyle changes, and the necessary treatment options available, including medication.
Types of Osteomalacia:
a) Nutritional Osteomalacia:
This type of osteomalacia arises from an inadequate intake of vitamin D or calcium-rich foods. It often affects individuals with poor diets or those who are unable to absorb nutrients properly.
b) Renal Osteomalacia:
Individuals with kidney disorders, such as chronic kidney disease, may develop renal osteomalacia. The kidneys play a crucial role in activating vitamin D, and when they are impaired, it can lead to decreased vitamin D levels and subsequent bone abnormalities.
c) Tumor-Induced Osteomalacia:
This rare form of osteomalacia occurs due to tumors, typically benign, that produce a hormone called fibroblast growth factor 23 (FGF23). This hormone inhibits the reabsorption of phosphate by the kidneys, leading to low levels of phosphate in the blood, which contributes to bone softening.
Reasons Behind Osteomalacia:
The primary cause of osteomalacia is a deficiency of vitamin D, which plays a vital role in maintaining bone health. There are several factors that can contribute to a deficiency of this essential vitamin:
a) Inadequate Sun Exposure:
Sunlight is a crucial source of vitamin D synthesis in the body. People who live in regions with limited sunlight, spend most of their time indoors, or wear clothing that covers most of their skin are more susceptible to vitamin D deficiency.
b) Poor Diet:
Individuals with a diet low in vitamin D and calcium-rich foods, such as fatty fish, dairy products, and fortified cereals, are at a higher risk of developing osteomalacia.
c) Malabsorption Issues:
Certain medical conditions, such as celiac disease, Crohn's disease, or gastric bypass surgery, can impair the absorption of vitamin D and other nutrients required for bone health.
Symptoms of Osteomalacia:
The symptoms of osteomalacia can vary in severity and may include:
a) Bone Pain:
Dull, aching bone pain is a common symptom, often affecting the lower back, hips, and legs. The pain may worsen at night or with weight-bearing activities.
b) Muscle Weakness:
Osteomalacia can lead to generalized muscle weakness, making it difficult to perform daily activities.
c) Bone Fractures:
Weakened bones are more susceptible to fractures, even with minor trauma or normal physical activity.
Prevention and Coping Strategies:
Preventing and managing osteomalacia involves adopting certain lifestyle changes and incorporating healthy habits:
a) Adequate Sun Exposure:
Spend time outdoors in sunlight, especially during the early morning or late afternoon when the sun's rays are less intense. Aim for about 10-15 minutes of sun exposure on your face, arms, and legs without sunscreen several times a week.
b) Balanced Diet:
Include foods rich in vitamin D and calcium in your diet. This includes fatty fish (salmon, mackerel), fortified dairy products, eggs, mushrooms, and leafy green vegetables. Consider talking to a healthcare professional about the need for vitamin D or calcium supplements.
c) Regular Exercise:
Engage in weight-bearing exercises like walking, jogging, or dancing to improve bone density and muscle strength. Consult with a healthcare professional or a physical therapist to design an exercise routine suitable for your condition.
d) Vitamin D Supplements:
In cases of severe deficiency or specific medical conditions, healthcare providers may recommend vitamin D supplements to ensure adequate levels in the body.
Necessary Treatment Options:
When lifestyle changes alone are insufficient, healthcare providers may recommend specific treatments for osteomalacia:
a) Vitamin D Supplements:
The primary treatment for osteomalacia involves vitamin D supplementation. This can be in the form of vitamin D3 (cholecalciferol) or vitamin D2 (ergocalciferol), depending on the individual's needs.
b) Calcium Supplements:
In addition to vitamin D, calcium supplements may be prescribed to ensure optimal bone health. It is essential to follow healthcare providers' instructions regarding dosage and timing.
c) Underlying Condition Treatment:
If osteomalacia is secondary to an underlying condition, such as kidney disease or malabsorption disorders, treating the primary condition is crucial to managing osteomalacia effectively.
Conclusion:
Osteomalacia, a condition characterized by weakened and soft bones, can significantly impact an individual's quality of life. By understanding the different types, causes, and symptoms of osteomalacia, along with adopting preventive measures and coping strategies, individuals can actively manage the condition. Lifestyle changes, including adequate sun exposure, a balanced diet, regular exercise, and appropriate supplementation, coupled with necessary medical treatments, play a crucial role in preventing and mitigating the effects of osteomalacia. If you suspect you may have osteomalacia or are experiencing symptoms, consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
Note: This article is for informational purposes only and should not replace any professional medical advice.









0 Comments